What is muscle atrophy?
Muscle atrophy refers to a decrease in muscle volume. More specifically, it refers to the striated muscles of the skeleton, muscles that are under voluntary control.

Muscle Atrophy. Image Courtesy of OpenStax
The characteristics of atrophy are variable. Depending on the case, this muscle atrophy can be:
- Localized or generalized, meaning it can affect a single muscle, all the muscles in a muscle group, or all the muscles in the body.
- Acute or chronic, with rapid or progressive development.
- Congenital or acquired, i.e., it may be caused by an abnormality present from birth or be the result of an acquired disorder.
What are the causes?
Muscle Atrophy can have different causes. It may be due to:
- Physical immobilization, i.e., prolonged immobilization of a muscle or muscle group.
- Hereditary myopathy, a hereditary disease that affects the muscles.
- Acquired myopathy, a disease of the muscles whose cause is not hereditary.
- A deterioration of the nervous system.
Physical immobilization
Physical immobilization can lead to atrophy due to a lack of muscle activity. Immobilization of muscles may be caused, for example, by the application of a cast to a fracture. This atrophy, sometimes called muscle atrophy, is benign and reversible.
Hereditary myopathy
Myopathies of hereditary origin may also be the cause of atrophy. This is especially true for several muscular dystrophies, diseases characterized by the degeneration of muscle fibers.
Hereditary causes of Muscular atrophy include:
- Duchenne muscular dystrophy, a rare genetic disorder characterized by progressive and widespread muscle degeneration.
- Steinert’s disease or Steinert’s myotonic dystrophy, a disease that can manifest as atrophy and myotonia (muscle tone disorder).
- Facioscapulohumeral myopathy, a type of muscular dystrophy that affects the muscles of the face and those of the shoulder blades (which connects the upper limbs to the trunk).
Acquired myopathy
Muscle Atrophy can also be a consequence of acquired myopathies. These muscle diseases are not hereditary and can have various causes.
Acquired myopathies may have an inflammatory origin, especially during :
- Polymyositis, which is characterized by inflammation of the muscles.
- Dermatomyositis, which is characterized by inflammation of the skin and muscles.
Acquired myopathies can also be non-inflammatory in nature:
This is especially true for myopathies of iatrogenic origin, i.e., muscle disorders resulting from medical treatment. For example, cortisone and its derivatives can cause atrophy in high doses and over the long term. Muscle atrophy can also be a symptom cachexia and diabetes.
Neurological causes of atrophy
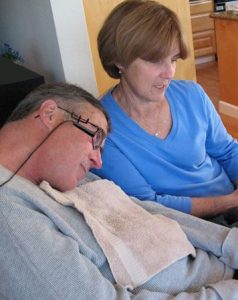
A Man With ALS
In some cases, atrophy may have a neurological origin. Muscle atrophy is due to damage to the nervous system.
There are several possible explanations for this, including the following:
- Amyotrophic lateral sclerosis (Lou Gehrig’s disease/Charcot disease) is a neurodegenerative condition that affects motor neurons (nerve cells involved in movement) and causes atrophy and then progressive paralysis of muscles.
- Spinal muscular atrophy, a rare genetic disorder that can also affect the muscles.
- Polio, an infectious disease of viral origin (poliovirus) that can cause myotropic and paralytic conditions.
- Nerve damage, which can occur to one or more nerves.
what is the risk of complications?
The progression of muscle atrophy depends on many parameters, including the cause, the patient’s condition, and medical treatment. In some cases, the atrophy may worsen and spread to other muscles in the body or even to the whole body. In the most severe forms, muscle atrophy may be irreversible.
How is Muscle Atrophy treated?
Treatment consists of treating the cause of the atrophy. For example, medications may be used to treat inflammatory myopathy, diabetes and cachexia. Physical therapy sessions may be recommended for prolonged physical immobilization.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5069191/
https://www.sciencedirect.com/topics/veterinary-science-and-veterinary-medicine/amyotrophy
FEEDBACK:



